Rotator Cuff Tear Arthropathy
|
||||||
Introduction
Physical therapy in Seattle for Rotator Cuff Tear Arthropathy
Welcome to Core Physical Therapy's guide on Rotator Cuff Tear Arthropathy.
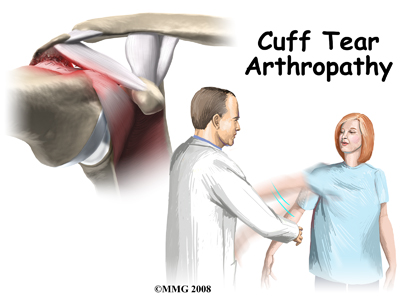
The rotator cuff is a unique structure in the shoulder that is formed by four tendons. These four tendons attach to four muscles that help keep the shoulder stabilized in the shoulder socket and help rotate the upper arm inward and outward. If the rotator cuff is severely torn and is not repaired, a type of arthritis of the shoulder may develop over time, which is termed rotator cuff arthropathy. The prefix ‘arthro’ means joint and ‘pathy’ means disorder therefore in simple terms, a ‘joint disorder’ develops. If you develop rotator cuff arthropathy your shoulder will be painful and movement and strength of the shoulder will be decreased. Moving the arm away from the body and raising it over your head can be particularly difficult.
This guide will help you understand:
- what parts of the shoulder are involved
- what causes this condition
- how healthcare professionals diagnose this condition
- what treatment options are available
- what Core Physical Therapy’s approach to rehabilitation is
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Shoulder Pain|limit:15|heading:Hear from some of our patients who we treated for *Shoulder Pain*#
Anatomy
What parts of the shoulder are involved?
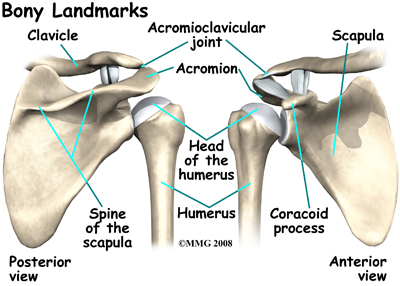
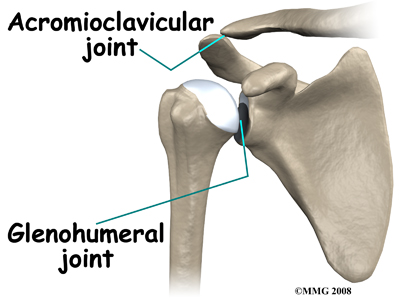
The shoulder joint is also called the glenohumeral joint. The shoulder joint is made up of three bones; the humerus (the upper arm bone), the scapula (the shoulder blade), and the clavicle (the collar bone).
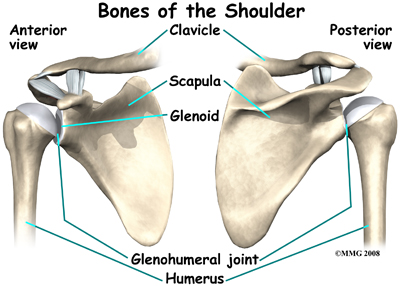
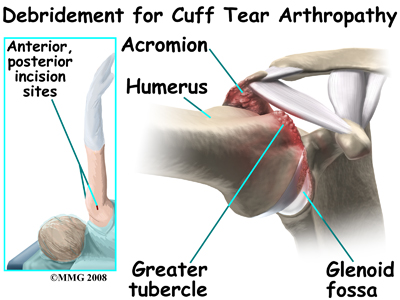
The humerus bone has a ball, called the humeral head, on the top end of it. The humeral head fits into a small, shallow cup called the glenoid fossa (shoulder socket). The glenoid fossa is part of the shoulder blade bone (the scapula). The roof of the glenoid fossa is also formed by a part of the scapula called the acromion.
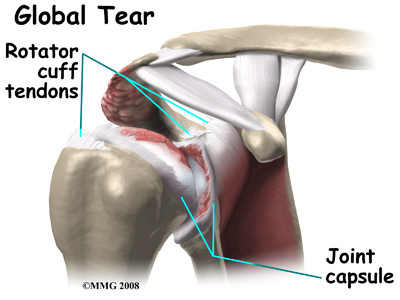
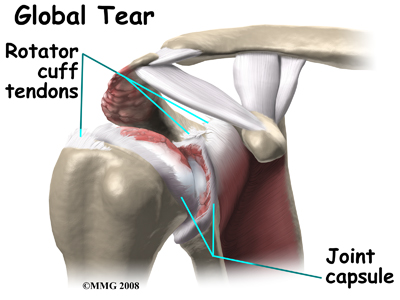
The rotator cuff is made up of tough, fibrous tissue. It forms a cuff (or capsule) covering the shoulder joint. There are four tendons that help form the rotator cuff. Tendons attach muscles to bones. Muscles move the bones by pulling on the tendon that they attach to. The rotator cuff muscles help raise and rotate the arm. As the arm is raised, the rotator cuff also keeps the humerus tightly in the socket.
The muscles that attach to the cuff tendons are the supraspinatus, infraspinatus, teres minor, and subscapularis. These muscles rotate the shoulder outward and inward. Along with another muscle, the deltoid, they also help lift the arm away from the body.
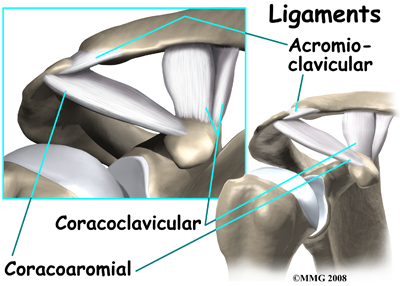
As mentioned above, the socket of the shoulder is part of the scapula bone and is called the glenoid fossa. The glenoid fossa is very shallow and flat so without the rotator cuff muscles the top part of the humerus (the humeral head) would slide out of the centre of the fossa as it moves.
As we raise our arm, part of the rotator cuff slides between the humeral head and the acromion. This sliding occurs over and over during everyday use. The rotator cuff tendons can be pinched in this space due to a number of reasons, including altered biomechanics from an injury or simply from repetitive use. This pinching is called impingement. Over time this pinching can lead to damage and weakening of the rotator cuff tendons, and an eventual fraying or tearing of them.
Related Document: Core Physical Therapy's Guide to Shoulder Anatomy
Related Document: Core Physical Therapy's Guide to Rotator Cuff Tears
Causes
What causes this condition?
Dr. Charles Neer described rotator cuff tear arthropathy in 1977. Today, doctors generally refer to this as simply cuff tear arthropathy. Cuff tear arthropathy is actually a type of ‘wear and tear’ degenerative arthritis of the shoulder that develops over time after the rotator cuff is damaged.
Normally, when the rotator cuff muscles contract, they pull the head of the humerus tightly into the socket of the shoulder. This stabilizes the shoulder and allows the large deltoid muscle to raise the arm over the head as it rotates the humeral head like a pulley. This motion needs the rotator cuff and deltoid muscles to work together in balance, in order for proper biomechanics to occur.
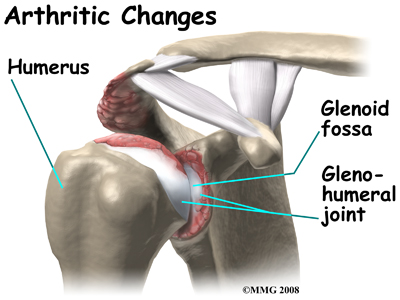
When the rotator cuff is torn, the shoulder becomes unbalanced. The deltoid muscle pulls the head of the humerus up into the acromion in a sliding motion rather than in the smooth balanced movement that the shoulder was designed to undergo. Over time this abnormal sliding motion causes wear and tear on the joint surfaces, which is termed arthritis. Due to the arthritis, motion of the shoulder becomes painful and the shoulder becomes weaker and weaker until you can no longer raise the arm above the head.
Rotator cuff tears are very common. Rotator cuff damage can occur from a single traumatic injury, such as a fall, lifting something heavy, or pulling forcefully. Most often, however, damage to the rotator cuff occurs gradually. Age can be a factor in this degeneration. As we age, the tendons of the rotator cuff become weaker and are more likely to be injured. In addition, with age, the blood supply to the tendons diminishes so any damage that does occur does not heal as well. Rotator cuff tears are much more likely to occur after the age of 40.
Certain activities can increase the wear and tear on the rotator cuff. For example repetitive overhead activity such as painting, plastering, racquetball, weightlifting, and swimming can all cause wear-and-tear of the rotator cuff.
Surgeons will generally recommend surgery to repair a severe rotator cuff tear when it occurs. A successful surgical repair of a torn rotator cuff tear can make the development of cuff tear arthropathy much less likely. Sometimes, however, a rotator cuff tear cannot be repaired. The tissue is simply too damaged and cannot be fixed. This is common in older patients with rotator cuff tears. In other situations, although possible to repair, the patient elects not to have surgery to fix the rotator cuff tear and chooses to simply live with the discomfort and limitations it may impose. Over several years, both of these situations can result in the eventual development of rotator cuff arthropathy.
Symptoms
What does this condition feel like?
The most common symptom of rotator cuff tear arthropathy is pain in and around the shoulder. The pain can also radiate into your neck or arm, and even into your wrist or hand. The pain is usually worse at night and can interrupt your sleep, especially if you try to sleep on the affected shoulder. The shoulder is often particularly painful when trying to lift the arm, or rotate it outward. If untreated, the pain can be severe and nearly continuous.
Weakness of the shoulder due to arthropathy makes it difficult, and nearly impossible, to lift the arm overhead. Often even starting the lifting motion can be difficult and for this reason, the tendency is to shrug your shoulder upwards in order to be able to lift the arm part of the way. Over time, the weakness of the rotator cuff muscles gets worse and range of motion can become quite limited. Routine things, like reaching behind your back, reaching into a cabinet, or combing your hair become difficult. You may notice a crackling or popping sensation coming from your shoulder blade area, which develops due to the altered mechanics in this area of the shoulder. When there is arthritis of the glenohumeral joint, there is often an associated creaking or grating sound inside the joint.
Diagnosis
How do healthcare professionals diagnose this condition?
Your healthcare professional will conduct a thorough history and carry out a clinical exam in order to determine that your problem is due to rotator cuff arthropathy. Your healthcare professional will inquire about when your pain started and if it occurred due to a specific injury or whether it came on gradually. They will also ask you about general activities that may have injured your shoulder and will also want to know about what makes your pain better or worse. In addition, your healthcare professional will want to know the level of your pain, and what activities in your daily life are limited by your shoulder injury.
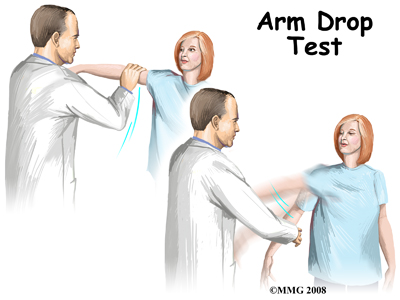
Next your healthcare professional will do a physical examination. Firstly, they will look at your shoulder to see if there are any bony deformities, or if there is any atrophy (wasting) of your muscles. They will feel your shoulder to determine which area is most painful for you. Next they will assess the range of motion of your shoulder and will also assess the strength of your shoulder and shoulder blade muscles. Your healthcare professional will also check to see how stable your shoulder is in the shoulder socket.
As mentioned above, with a complete rotator cuff tear, moving the arm away from the body can be nearly impossible. A common test to be done when there is suspicion of a rotator cuff tear is the Drop Arm Test. For this test your healthcare professional lifts your affected arm for you and asks you to hold it there. If you cannot hold it up, this test is considered positive and usually indicates that the rotator cuff is torn.
Other areas such as the neck will also be evaluated for range of motion and strength. A pinched nerve in the neck can mimic a rotator cuff tear. A neurological examination, which includes checking your reflexes and sensation, may also be included.
Investigations
What investigations will need to be done?
Your healthcare professional will request X-rays of your shoulder. X-rays show the shape and positioning of your bones and joints. When the rotator cuff is torn, the shoulder will often ride high, meaning that it sits higher in the joint than it should. An X-ray can also show how much damage has occurred to the joint surfaces.
You may be asked to have an electromyogram (EMG), which checks the function of the muscles of the shoulder. An EMG uses a small needle in the muscle being tested. It measures the electrical activity of the muscle at rest, and when tightened.
Magnetic resonance imaging (MRI) allows your healthcare professional to look at slices of the area in question. The MRI machine uses magnetic waves, not X-rays, to show the muscle, tendons, and ligaments of the shoulder. MRIs will show tears of the rotator cuff tendons. Atrophy of the muscles can also be evaluated with MRI.
A computerized tomography (CT) scan shows slices of bone. Like X-rays, this test uses radiation. A CT scan can help to more accurately determine the degree of damage of the glenohumeral joint. A CT scan is especially useful to plan for surgery if a surgery is considered for treatment.
Treatment
What treatment options are available?
Nonsurgical Treatment
Conservative care for arthropathy includes physical therapy as well as oral anti-inflammatories. A corticosteroid injection into the shoulder joint is also sometimes helpful. Steroids are very powerful anti-inflammatory medications that can reduce pain temporarily. These injections will not heal the original tear but may give pain relief for several weeks to months, and may allow you enough pain-free time to assist with making gains during rehabilitation. The goal of conservative treatment is to reduce pain, and increase range of motion and function.
Nonsurgical Rehabilitation
Physical therapy at Core Physical Therapy can be very helpful if you are suffering from rotator cuff arthropathy.
The goal of physical therapy is to decrease your pain, and improve your range of motion, strength, and overall function as much as possible. Preventing further wear-and-tear on your joint is also an important goal.
As an initial treatment your therapist may use modalities such as heat, ice, ultrasound, or electrical current to assist with decreasing any pain or swelling you have around your shoulder, or anywhere along your arm, or into your hand. Due to some of the muscles of the neck and upper back connecting to the shoulder, you may also have pain in these regions, which your therapist can treat in order to make movement of your entire upper body easier. Your therapist may also use massage or mobilizations for your neck, upper back, shoulder, shoulder blade, elbow, or wrist in order to improve circulation and assist with any pain that may be present.
Next your therapist will focus on your range of motion. The exercises they prescribe will focus on the ranges of motion that are most limited as well as those which are most useful to your overall daily functioning. Your therapist may encourage the use of poles or pulleys in order to gain passive range of motion of your shoulder without causing any pain. Passive range of motion helps provide nutrition to the joint and stretch the muscles and tissues of the joint into ranges that you are unable to achieve by using your own muscle strength. Your therapist may also assist your range of motion by mobilizing your shoulder joint or shoulder blade or assisting with some specific range of motion stretches. Other areas such as your neck, elbow, or upper back may also become stiff as a result of dealing with a rotator cuff arthropathy. When necessary your therapist will mobilize these areas and also prescribe exercises to assist with range of motion for these areas.
In addition to range of motion exercises, strengthening exercises will be prescribed. These exercises may include the use of rubber bands or tubings, weight machines, free weights, or they may simply make use of your own body weight. In order to function properly and avoid further injury, both the strength of the muscles supporting the shoulder joint (the rotator cuff) as well as the strength of the muscles around the shoulder blade (scapula) need to be adequate.
Proprioception is the ability to know where your body is without looking at it. As a result of any injury or surgery, this ability declines in function. A period of decreased joint mobility adds to this decline. Although your arm and shoulder girdle are not traditionally thought of as weight-bearing parts of the body, even an activity such as assisting yourself with your arms to get out of a chair or pulling a glass from a cupboard requires weight through your shoulder girdle and for your body to be proprioceptively aware of your limb.
The proprioceptive control of the scapula on the rib cage (scapulothoracic motion) is especially important in being able to use your shoulder girdle and upper limb effectively without causing further injury to your shoulder. For this reason, your physical therapist will teach you how to properly control your scapula during your rehabilitation exercises as well as during everyday activities. Proprioceptive exercises might include activities such as rolling a ball on a surface with your hand, holding a weight up while moving your shoulder, or doing push-ups on an unstable surface. Advanced exercises may include activities such as ball throwing or catching. As often as possible exercises that simulate your everyday activities such as grooming yourself and getting dressed, in addition to those activities that simulate your work or hobbies will also be incorporated.
Regaining proprioception of the shoulder girdle and upper limb can require concentrated work, and most people have not previously needed to focus so intently on such controlled motions of this joint. The concentrated effort of shoulder rehabilitation, however, has a substantial reward; good scapulothoracic control is the key to regaining maximum shoulder range of motion and thus improved shoulder functioning while avoiding future pain.
As part of your rehabilitation your therapist may choose to use tape on your shoulder joint or your shoulder girdle in order to assist with your pain. Taping the shoulder can also assist with proprioception of the joint.
Your physical therapist will also remind you about maintaining good shoulder posture when sitting or using your upper limb in activities below shoulder height, such as working on the computer. Rounded shoulders in this position crowds the shoulder joint and can lead to shoulder impingement and pain. Excellent posture is also required when doing activities at or above shoulder height in order to avoid further injury. Your therapist will also discuss ways you can protect your shoulder during daily activities and show you ways to move in order to avoid causing more damage to your joint.
Sometimes, even with conservative treatment, your pain remains continuous and severe, and your range of motion remains significantly limited. In these cases your therapist may refer you to an orthopaedic surgeon as surgery may need to be considered as a treatment option.
Core Physical Therapy provides services for physical therapy in Seattle.
Surgery
What surgery can be done to help?
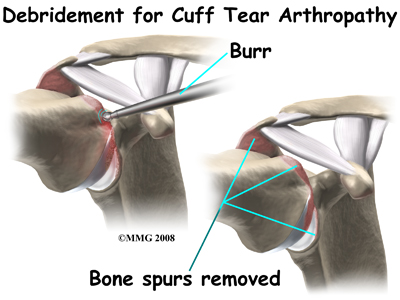
Surgery for cuff tear arthropathy is done when pain and decreased motion continue even after trying conservative care. As indicated previously, cuff tear arthropathy is the result of a long-standing lack of rotator cuff function. For this reason, in almost all cases, surgical repair of the rotator cuff tear is no longer an option. The simplest surgical procedure to try and improve the situation is a debridement. During a debridement, the surgeon will surgically remove (debride) any inflamed tissue, bones spurs and loose flaps of tendon tissue that may be catching in the joint and causing pain. This procedure may reduce pain, however, it does not always improve range of motion, strength, or function of the shoulder.
Patients with rotator cuff arthropathy would seem to be good candidates for a shoulder replacement, but unfortunately replacing the shoulder in the typical fashion has not been successful. Replacing the shoulder with a special type of artificial shoulder joint, however, is becoming more popular. This procedure is called a reverse shoulder replacement.
The traditional shoulder replacement was designed to simulate our real shoulder. The glenoid component of the replacement (the socket) was designed to replace our normal shoulder socket by using a thin, shallow plastic cup. The humeral head component was designed to replace the ball of the humerus by using a metal ball that sits on top of the glenoid. This situation has been compared to placing a ball on a shallow saucer. Without ‘something’ to hold the metal ball in place, the ball simply slides around on the saucer. In a normal shoulder that ‘something’ is the rotator cuff and the rotator cuff muscles. With a traditional shoulder replacement it was found that without a rotator cuff to hold the metal ball centered in the plastic socket, no meaningful movement could be accomplished. Unfortunately the metal quickly wore out the plastic socket, and the joint became painful once again. Even the large deltoid muscle, in this type of shoulder replacement, is unable to assist enough without a rotator cuff in order to produce any useful motion of the shoulder.
Due to this ‘no rotator cuff’ dilemma the mechanics of the shoulder joint needed to be reconsidered and a design for an artificial shoulder that worked differently than the real shoulder joint needed to be created. The solution that evolved was to reverse the socket and the ball, placing the ball portion of the shoulder where the socket use to be and the socket where the ball or humeral head use to be. This new design has led to a much more stable shoulder joint that can function much better without a rotator cuff. The artificial joint itself provides more stability to the shoulder by creating a deeper socket that prevents the ball from sliding up and down as the shoulder is raised. The large deltoid muscle that covers the shoulder can be used more effectively to lift the arm, which provides better functional use of the shoulder. The final result is a shoulder that functions better, is less painful and can last for years without loosening.
Related Document: Core Physical Therapy's Guide to Reverse Shoulder Arthroplasty
Post-surgical Rehabilitation
What should I expect after surgery?
What you do for post-surgical rehabilitation depends on what type of surgery you have had. Those who have had a surgical debridement will require much less intense therapy than those who have had a full reverse shoulder arthroplasty. No matter which type of surgery you undergo, you will most likely require the use of a sling or shoulder brace after the surgery to protect your joint while it heals.
Generally after any type of surgery for rotator cuff arthropathy, a physical therapist will see you in the hospital the day after surgery to begin your rehabilitation program. Your therapist will make sure you are safe when getting in and out of bed and moving about in your room with your sling on. Next, if your surgeon allows it, they will prescribe specific range of motion exercises for you. Your therapist will teach you how to remove your sling for your exercises and also how to put it back on after you have completed your exercises. After a major surgery such as the reverse shoulder replacement the sling should be worn at all times except during showering and while performing rehabilitation exercises.
When the immobilizer is removed following surgery, you will experience some pain when you start to move your shoulder, wrist, elbow and forearm. This pain is normal and is from not using the joints very efficiently previous to the surgery and also from the surgical process itself. The pain you feel with movement should only be mild to moderate and any sharp or severe pain should be heeded. In addition, after surgery the muscles in your arm may appear small and atrophied. Again, this is normal; once your strength begins to return your arm will start to look more normal again.
Simple finger, hand and wrist movements, as well as elbow and neck range of motion exercises will be prescribed to ensure you regain motion in these joints. Pendular exercises for your shoulder will be prescribed along with passive range of motion exercises that encourage shoulder elevation (raising in front) as well as gentle external rotation. Pendular exercises are performed by leaning forward or to the side, letting the arm hang clear of the chest, and then initiating movement with your trunk so that the dangling limb passively and gently moves. These exercises assist with pain, help to maintain some shoulder range of motion, and assist in preventing unwanted scar tissue forming in the joint. This pendular action also provides some traction to the glenohumeral joint, which aids in pain relief, and also assists the shoulder into a relatively elevated motion (in relation to the trunk). It is important that the pendular activity is done as passively as possible without initiating motion from the shoulder muscles. This exercise should be similar to a weighted pendulum that randomly swings on the end of a piece of string. Icing your shoulder will be encouraged after your exercises as well as several other times during the day.
Once you are managing your exercises well in the hospital, you are independent in doing most activities to care for yourself, and when your surgeon feels it is appropriate, you will be sent home. You will need to continue an extensive rehabilitation program once you are discharged from the hospital. In some cases, a physical therapist or occupational therapist may visit your home to check to see that you are safely getting around within your home and managing your everyday tasks with your arm in your sling. Your therapist may also review and assist you with your exercises at this time. If it is particularly difficult for you to get out of your home to attend physical therapy at Core Physical Therapy then a physical therapist may continue to visit you at your home for several treatments in order to review and advance your exercises. As soon as you are able, however, it is best for you to attend rehabilitation at Core Physical Therapy as there are several more modalities as well as exercise equipment that can be used in the clinic versus at home, which can expedite your recovery.
As an initial goal of rehabilitation your physical therapist at Core Physical Therapy will focus on relieving your pain and decreasing any swelling that may be lingering from the surgery. We may use modalities such as heat, ice, ultrasound, or electrical current to assist with pain or decrease any swelling you have around your shoulder, anywhere along your arm, or into your hand. Due to some of the muscles of the neck and upper back connecting to the shoulder, you may also have pain in these regions, which we can also treat in order to make movement of your entire upper body easier. We may also use massage or mobilizations for the neck, upper back, shoulder, elbow, forearm, or wrist to improve circulation and assist with any pain that may be present.
If a reverse shoulder replacement has been done then protecting the new joint is of particular importance. Due to the biomechanics of a reverse arthroplasty there is a higher risk of shoulder dislocation than after a traditional shoulder replacement. With a traditional shoulder replacement the shoulder is more likely to dislocate with the arm in abduction and external rotation. With the reverse shoulder replacement dislocation is most likely during isolated extension as well as the combined movements of extension, internal rotation, and adduction therefore these movements should be avoided. Your therapist will review these movement precautions with you and you should refrain from putting your shoulder in any of these positions on their own or in combination for a minimum of 12 weeks post-surgically. Activities involving these positions, such as tucking in one’s shirt or performing personal hygiene of the back passage, are simple activities but can lead to dislocation so they must be strictly avoided. It can be helpful in respecting these precautions by remembering that you should always be able to see the elbow on your surgical side during all activities with that arm.
The next part of our post-surgical treatment will focus on regaining the range of motion, strength, and dexterity in your shoulder, elbow, hand and wrist. Your physical therapist at Core Physical Therapy will prescribe a series of stretching and strengthening exercises that you will practice in the clinic and also learn to do as part of your home exercise program. These exercises may include the use of rehabilitation equipment such as pulleys and poles for range of motion exercises, and light weights or exercise bands for resistance work of your upper limb. The shoulder joint is the upper limb’s link to the rest of the body so it needs to be strong and well controlled for the limb and hand to work properly. If you have access to a pool your therapist may suggest you do some of your rehabilitation exercises in the pool where the warmth of the water and the hydrostatic properties of the water can be of assistance.
As time and range of motion progress, strengthening will become the major focus and will be advanced so that heavier weights or elastic bands are used and endurance of the muscles is improved. Your therapist will monitor your progress and advance your exercises as your shoulder can tolerate them. Along with more advanced strengthening exercises, active range of motion of the shoulder will be encouraged in order to assist with strengthening and control of the entire shoulder girdle.
Proprioception is the ability to know where your body is without looking at it. As a result of any injury or surgery, this ability declines in function. A period of immobilization adds to this decline. Although your arm and shoulder girdle are not traditionally thought of as weight-bearing parts of the body, even an activity such as assisting yourself with your arms to get out of a chair or pulling a glass from a cupboard requires weight to be put through or lifted by your shoulder girdle and for your body to be proprioceptively aware of your limb.
The proprioceptive control of the scapula on the rib cage (scapulothoracic motion) is especially important in being able to use your shoulder girdle and upper limb effectively without causing further injury. For this reason, your physical therapist will teach you how to properly control your scapula during your rehabilitation exercises as well as during everyday activities. Your physical therapist will also remind you about maintaining good shoulder posture at all times even when sitting or using your upper limb in activities below shoulder height, such as working on the computer. Rounded shoulders in this position crowds the shoulder joint and can lead to shoulder impingement and pain.
Regaining proprioception of the shoulder girdle and upper limb can require concentrated work, and most people have not previously needed to focus so intently on such controlled motions of this joint. The concentrated effort of shoulder rehabilitation, however, has a substantial reward; good scapulothoracic control is the key to regaining maximum shoulder girdle control and improved shoulder functioning while avoiding future shoulder pain.
Proprioceptive exercises might include activities such as rolling a ball on a surface with your hand, holding a weight up while moving your shoulder, or push-ups on an unstable surface. Advanced exercises may include activities such as ball throwing or catching. Exercises that simulate your everyday activities such as grooming yourself and getting dressed, in addition to those activities that simulate your work or hobbies will also be incorporated.
At Core Physical Therapy we also highly recommend maintaining the rest of your body’s fitness with regular exercise while recovering from surgery. Several types of cardiovascular machines can be used such as a stationary bike, a stepper, or a treadmill for walking. Cardiovascular activity in a pool may also be appropriate. Your physical therapist at Core Physical Therapy can discuss when cardiovascular activity would be appropriate for you and which cardiovascular activity would be best. Most importantly, your surgical shoulder needs to be protected at all times so your therapist will educate you on how to do this.
Generally rehabilitation at Core Physical Therapy after surgery for rotator cuff arthropathy goes smoothly. If, however, during rehabilitation your pain continues longer than it should or therapy is not progressing as your physical therapist would expect, we will ask you to follow-up with your surgeon or doctor to confirm that the shoulder is tolerating the rehabilitation well and to ensure that there are no hardware issues that may be impeding your recovery.
Portions of this document copyright MMG, LLC.


